By: Sanah Ahsan
We are living, we’re told, through a “mental health crisis”. Mental health services cannot cope with the explosion of demand over the past two years: 1.6 million people are on waiting lists, while another 8 million need help but can’t even get on these lists. Even children are showing up at A&E in despair, wanting to die.
But there is another way to see this crisis – one that doesn’t place it firmly in the realm of the medical system. Doesn’t it make sense that so many of us are suffering? Of course it does: we are living in a traumatising and uncertain world. The climate is breaking down, we’re trying to stay on top of rising living costs, still weighted with grief, contagion and isolation, while revelations about the police murdering women and strip-searching children shatter our faith in those who are supposed to protect us.
As a clinical psychologist who has been working in NHS services for a decade, I’ve seen first hand how we are failing people by locating their problems within them as some kind of mental disorder or psychological issue, and thereby depoliticising their distress. Will six sessions of CBT, designed to target “unhelpful” thinking styles, really be effective for someone who doesn’t know how they’re going to feed their family for another week? Antidepressants aren’t going to eradicate the relentless racial trauma a black man is surviving in a hostile workplace, and branding people who are enduring sexual violence with a psychiatric disorder (in a world where two women a week are murdered in their own home) does nothing to keep them safe. Unsurprisingly, mindfulness isn’t helping children who are navigating poverty, peer pressure and competitive exam-driven school conditions, where bullying and social media harm are rife.
If a plant were wilting we wouldn’t diagnose it with “wilting-plant-syndrome” – we would change its conditions.
Yet when humans are suffering under unliveable conditions, we’re told something is wrong with us, and expected to keep pushing through. To keep working and producing, without acknowledging our hurt.
In efforts to destigmatise mental distress, “mental illness” is framed as an “illness like any other” – rooted in supposedly flawed brain chemistry. In reality, recent research concluded that depression is not caused by a chemical imbalance of the brain. Ironically, suggesting we have a broken brain for life increases stigma and disempowerment. What’s most devastating about this myth is that the problem and the solution are positioned in the person, distracting us from the environments that cause our distress.
Individual therapy is brilliant for lots of people, and antidepressants can help some people cope. But I worry that a purely medicalised, individualised understanding of mental health puts plasters over big gaping wounds, without addressing the source of violence. They encourage us to adapt to systems, thereby protecting the status quo. It is here that we fail marginalised people the most: Black people’s understandable expressions of hurt at living in a structurally racist society are too often medicalised, labelled dangerous and met with violence under the guise of “care”. Black people are more likely to be Tasered, sectioned, restrained and over-medicated than anyone else in our mental health services today.
The UK could learn a lot from liberation psychology. Founded in the 1980s by the Salvadorian activist and psychologist Ignacio Martín Baró, it argues that we cannot isolate “mental health problems” from our broader societal structures. Suffering emerges within people’s experiences and histories of oppression. Liberation psychology sees people not as patients, but potential social actors in the project of freedom, valuing their own lineages, creativity and experience, rather than being forced into a white, eurocentric and individualistic idea of therapy. It directly challenges the social, cultural and political causes of distress through collective social action.
This framework makes complete sense when we hear that the pandemic in the UK has affected poor people’s mental health most. Does it mean wealthy, privileged white men don’t experience suffering? Of course they do. We’re still learning about the complicated ways these structural issues affect our everyday lives. For example, how the pressures of individualism and capitalism may lead to isolation and substance abuse, or how colonial violence towards immigrant families plays out within homes and on bodies.
Let me be clear, I’m not saying people in distress should be out there on the picket line.
Pain can be debilitating. But those of us who are supporting people in distress, such as mental health workers, have a key role in social transformation. Social action is the medicine that relieves people’s personal and collective distress.
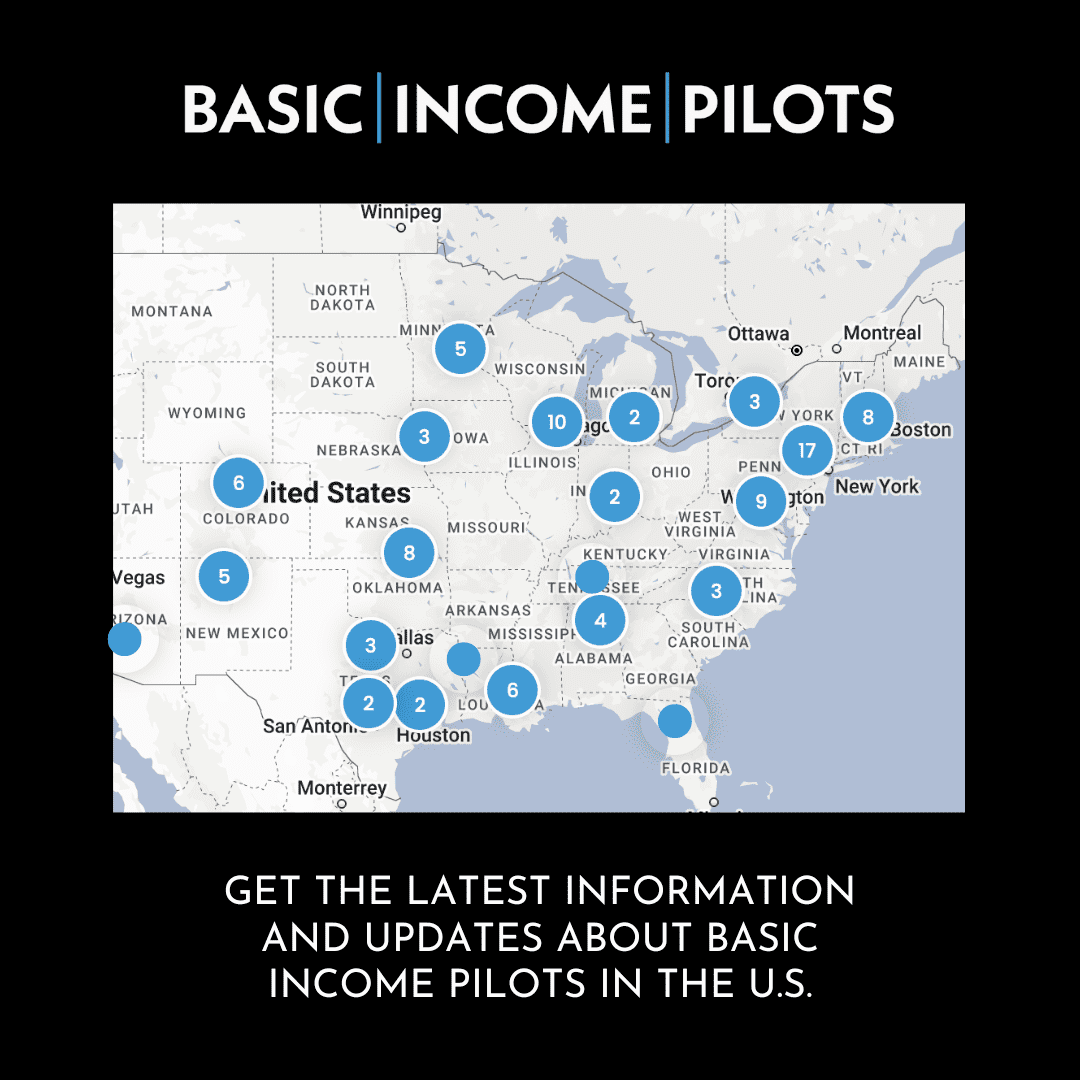
Instead of trying to change “mindsets” in therapy, we need to change race- and class-based hierarchies, the housing and economic system. Universal basic income has psychological benefits, and recent studies show how it improves the “crises of anxiety and depression”. As a clinical psychologist, some of my most powerful work has been not in the therapy room but in successfully advocating for secure housing for, or working in the community with, queer, black and brown facilitators in organisations such as Beyond Equality, to prevent gender-based violence. The network Psychologists for Social Change shows us a practical imagining of this work. We also need social change that is preventive, such as investing in young people and community-led services such as healing justice london and 4front. They work to shift trauma in marginalised communities through building social connectedness, social action and creativity, towards futures free of violence.
None of this is to dismiss the value of one-on-one therapy (that’s part of my job, after all). But therapy must be a place where oppression is examined, where the focus isn’t to simply reduce distress, but to see it as a survival response to an oppressive world. And ultimately, I’d like to see a world where we need fewer therapists. A culture that reclaims and embraces each other’s madness. Where we take the courageous (and sometimes skin-crawling) risk of turning to each other in our understandable, messy pain.
Meaningful structural transformation won’t happen overnight, though the pandemic taught us that big changes can happen pretty quickly. But change won’t happen without us: our distress might even be a sign of health – a telling indicator of where we can collectively resist the structures that are hurting so many of us.
To return to the plant analogy – we must look at our conditions. The water might be a universal basic income, the sun safe, affordable housing and easy access to nature and creativity. Food could be loving relationships, community or social support services. The most effective therapy would be transforming the oppressive aspects of society causing our pain. We all need to take whatever support is available to help us survive another day. Life is hard. But if we could transform the soil, access sunlight, nurture our interconnected roots and have room for our leaves to unfurl, wouldn’t life be a little more livable?