By: Maddie Bender
See original post here.
Give a man a fish, he’ll eat for a day. But give people no-strings-attached cash, and you’ll reduce the rate of new HIV infections and AIDS-related deaths. Cash transfer programs have become popular in low- and middle-income countries for their potential to provide social safety nets and alleviate poverty, but their primary goal isn’t to improve public health.
That’s why the findings of a new study, published Monday in Nature Human Behavior, are so encouraging for infectious disease scientists.
Researchers at the University of Pennsylvania analyzed over 20 years of data from cash transfer programs run in 42 different countries—not specifically developed to impact HIV and other STI infection, testing and treatment.
Aaron Richterman, an infectious disease researcher at the University of Pennsylvania and the lead author of the new study, told The Daily Beast he and his co-author distinguished these large-scale programs from smaller-scale experimental programs—the latter of which have shown mixed results at reducing HIV-related outcomes. Such studies may not account for two “spillover effects”: Cash recipients may share the money with their family, and infectious disease rates depend on the behaviors of an entire community, not just a subset of enrolled study subjects.
Getting tested for HIV and going on an effective treatment is “like a double whammy,” Richterman said. “It improves outcomes for that individual person, but it also improves outcomes for the community in terms of reducing transmissions to other people.”
Richterman stressed that the cash programs evaluated in the study were not meant to control HIV or other STIs, but the results demonstrate their utility to do so nonetheless. The programs corresponded with an immediate 6 percent reduction in the risk of a new HIV infection that continued up to a decade later. The risk of AIDS-related deaths decreased by 9 percent and HIV treatment coverage increased by 3 percent after a short delay.
“There are both economic pathways and psychological pathways” through which the programs can work, Richterman said.
Money can reduce barriers to get tested and afford medication, but it also can give individuals more mental bandwidth to focus on long-term decision-making.
Additionally, in sub-Saharan Africa, cash transfers may reduce the rate of transactional sex, which is a major HIV transmission risk factor for young women.
Most HIV reduction programs today focus on strictly public health measures, Richterman said, such as incentivizing high-risk individuals to take a pre-exposure prophylactic (PrEP) or get tested for HIV and other STIs. This study shows that “we should also think about a broader array of interventions, such as basic income,” he added.
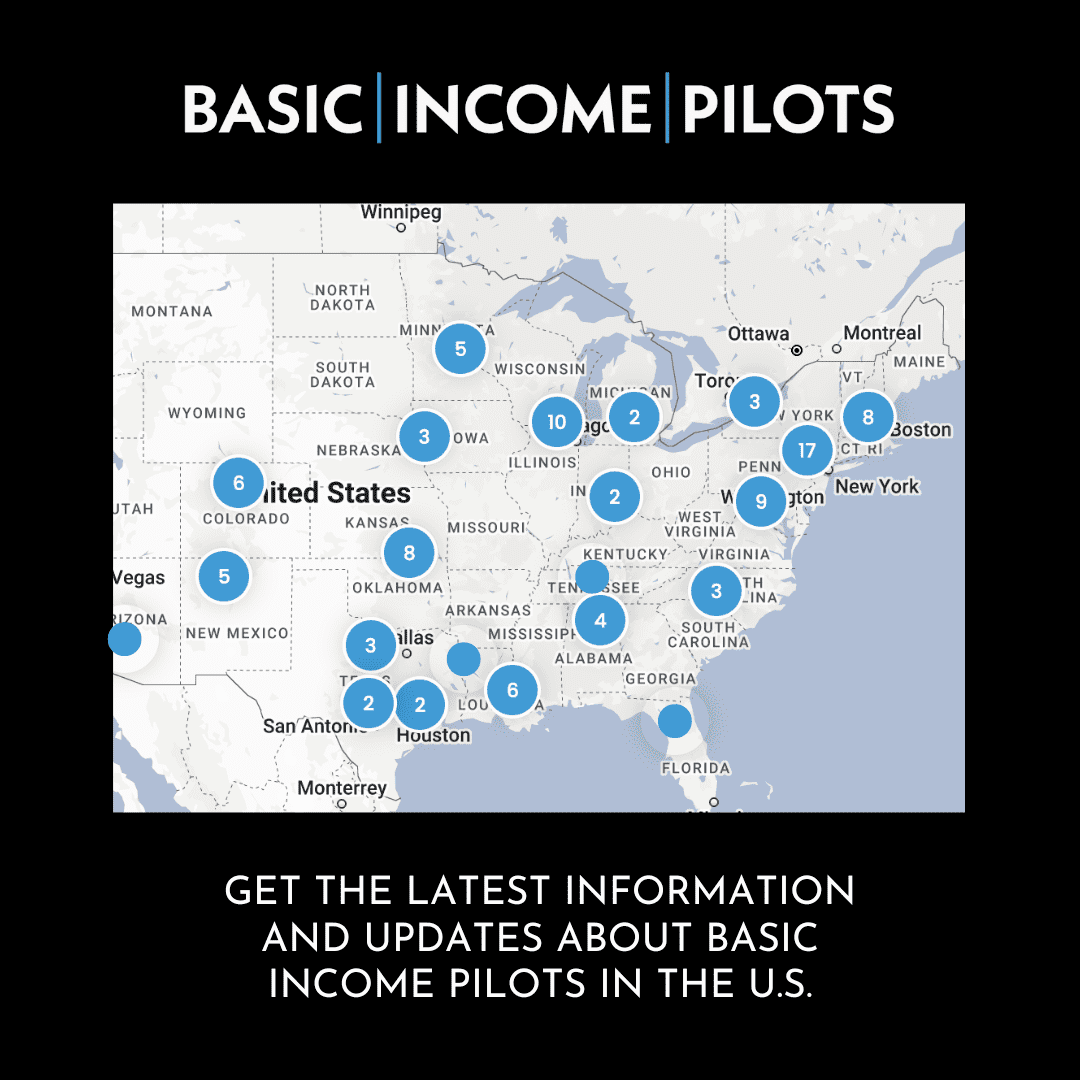
It’s not too much of a stretch to speculate about these findings in the context of proposed universal basic income plans in the United States. Richterman conducted another study that linked more generous SNAP benefits to a reduction in HIV rates. Even though the U.S. is considered a high-income country, his research has found that the major benefits to cash transfers seem to hold up.
“This is a country that has a great deal of inequality,” Richterman said. “It’s very plausible to start to think about how things like basic income could be used to end the HIV epidemic in the U.S.”