By: ELLIOTT JOHNSON and MATTHEW JOHNSON
Many older generations in the UK have experienced an economic sweet spot in the course of their lives in which excess demand for labour, technological development, distribution of state resources accumulated in the post-war period and relative peace resulted in higher salaries, greater opportunity and a rapidly increasing life expectancy. For the first time in several generations, younger people – particularly Millennials and Generation Z – have worse economic prospects than their parents. In their childhood and youth, they have faced financial meltdown, public health crises, major armed conflict and now a cost of living crisis. Even in times of relative stability, we have been rapidly travelling down a road of increased automation, concentration of wealth in the hands of fewer and fewer individuals, and decreasing opportunities for the least well-off to change their lives for the better. As the FT noted in September 2022 [paywalled article], ‘we are a poor country with some very rich people’.
Young people are feeling the consequences. As our RSA report, Challenging the mental health crisis: how universal basic income can address youth anxiety and depression, highlighted, young people’s rates of mental health problems, relative to previous cohorts and older people, are increasing and show no sign of abating. This report shows there is a strong association between the household incomes of young people and their likelihood of having symptoms of anxiety and depression. If you are from a lower household-income quintile background, you are more likely to have mental health problems. If that income changes throughout your childhood and adolescence, that risk changes too, for better or worse.
Delivering economic security
Greater investment in mental health services and innovation in treatments are clearly part of the solution. But what can we do to improve the conditions in which young people live to give them the best chance of making good on the government’s prevention agenda by avoiding ill health in the first place?
The answer, it appears, can no longer be found solely through top-line economic growth or trickle-down economics. This is precisely the approach that has worsened inequality, increased poverty, harmed the environment and reduced our health security overall. Aggregate growth has not improved the interests of the large portions of society who find themselves with lower real-term incomes than before the financial crisis.
Rather, we need to look to more radical solutions. Radical, here, does not mean reckless or incompatible with a flourishing, modern, liberal democratic order. Rather, it means no longer tinkering around the edges of economic policy. This has been tried. Universal Credit was an attempt to reform targeted and conditional benefits in a way that would deal with a poverty trap that disincentivised finding paid work. Despite these good intentions, it has failed disastrously with the use of food banks continuing to rise rapidly, even before the cost of living crisis.
Equity by another means
The history of our own nation, and the current circumstances in others, show that there is an alternative approach. Universal, equitable, cradle-to-grave forms of state support were responsible for bringing the UK out of the second world war as a prosperous, more equal and more empathic nation. They have also been responsible for Nordic countries maintaining both lower levels of inequality and greater GDP per capita than the UK. Good economics for the nation must not rely on bad finances for some. These expensive policies were introduced for short- and long-term benefit at a time in which our public budgets were most stretched, but when public need was greatest. We can either continue to decline or, as in the mid-20th century, embrace innovation and ambition.
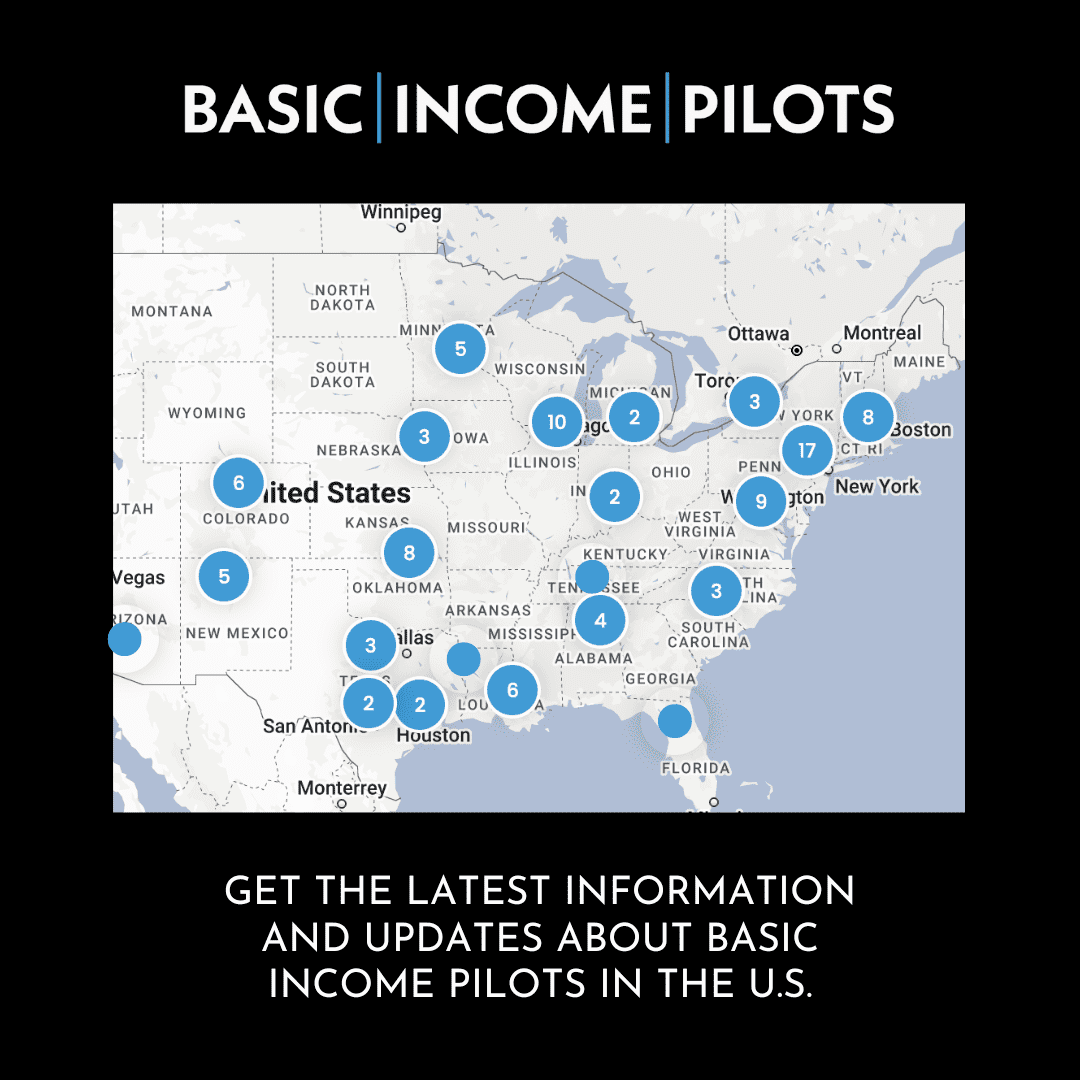
As our RSA report shows, a universal basic income (UBI) is feasible, affordable, has widespread public support and can help to address the rapidly worsening mental health of our young people. A trial of basic income for young care leavers is now under way in Wales, and NIHR-funded work is ongoing to establish the prospective scale of public health impact from the schemes set out in our report. There is a real chance to understand the broader health benefits that UBI could have across the population. This report is a starting point. We must strive to ensure that it is not an end in itself.