By Melissa Hellmann
See original post here.
A city’s infant mortality rate indicates the general health of a population, according to the Centers for Disease Control and Prevention.
That is especially the case in Philadelphia, which has the highest infant mortality and poverty rates among the nation’s 10 most populous cities. In their first year, Black infants die at more than triple the rate of white babies.
Throughout the U.S. in 2020, the leading causes of infant mortality included low birth weight and preterm birth. A guaranteed basic income for expectant parents can address those problems and even result in improved early childhood development, studies have shown.
So Philadelphia is doing just that: offering expectant parents unrestricted cash payments to improve birth outcomes and reduce racial disparities.
Beginning in 2024, the Philly Joy Bank will provide 250 pregnant Philadelphians with $1,000 a month in no-strings-attached cash throughout their pregnancy and for one year postpartum. Expectant parents who earn less than $100,000 annually and live in one of the city’s three neighborhoods with the highest percentages of low birth weight — majority Black neighborhoods — will be eligible for the program run by the Philadelphia Department of Public Health.
The Philly Joy Bank has received over $3.5 million in philanthropic funding from Spring Point Partners, the William Penn Foundation and the Barra Foundation. The program is also accepting donations. The city plans to fund an additional $750,000 in program administration.
Developed in partnership between the city’s Department of Public Health and the Philadelphia Community Action Network — a coalition focused on reducing infant mortality — the pilot program resulted from hours of conversations with local community members, as well as literature reviews of similar programs in Manitoba, Canada and San Francisco.
“We heard from Philadelphians not only that a program like this was sorely needed here, but that the amount of the monthly guaranteed income needed to be tied to a meaningful line item in a family’s monthly budget, such as housing or childcare,” said Stacey Kallem, Philadelphia Department of Public Health’s director of maternal, child, and family health division.
The $1,000 monthly benefit is based on the costs of local housing and childcare. Doula support, financial coaching and maternal and child home visits were also requested during community focus group sessions.
The rise of basic income
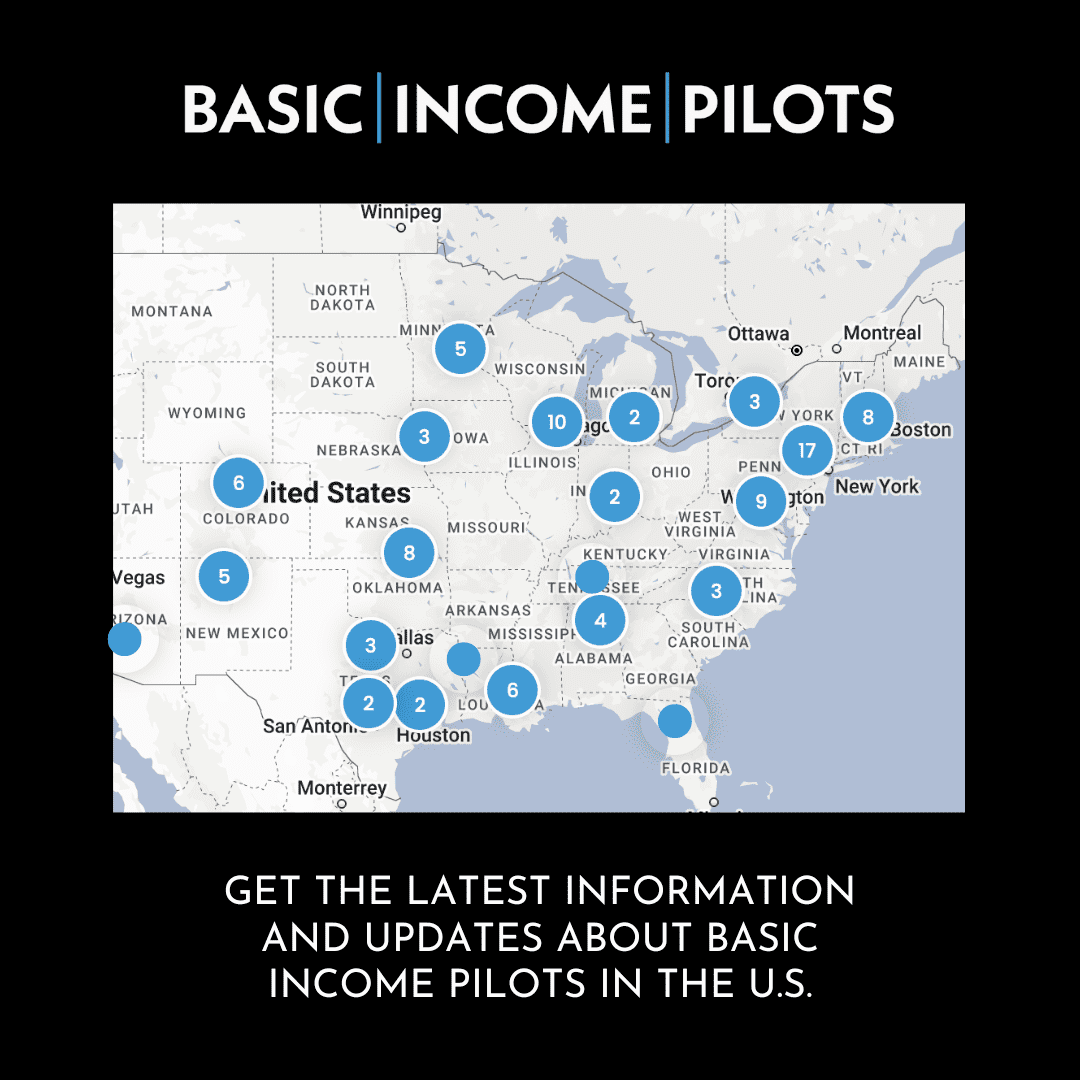
Guaranteed basic income experiments have increased in recent years as people search for solutions to growing income inequality that threatens wellbeing. Nearly 50 active guaranteed income programs exist throughout the U.S., according to Stanford Basic Income Lab, which conducts research and holds conversations on basic income. Those programs address a range of issues, including poverty and housing insecurity.
Data from more than 7,500 participants in basic income pilots throughout the nation show the greatest spending on retail sales and services at 40%, followed by food and groceries at 28%, according to Guaranteed Income Pilots Dashboard. Participants say the cash has allowed them to pay for medical bills, student loans, professional development, diapers and extra food on the table, among other expenses.
Critics of a general basic income argue that recipients will lose motivation to work. But years of research show that unrestricted cash helps people cover basic needs and can increase employment. A recent study on a basic income program in Stockton, California, revealed that $500 a month over 24 months resulted in improved mental health.
Philadelphia already tested the waters through several free cash programs in recent years, including a one-time $500 payment for formerly incarcerated people and a monthly payment averaging $890 to 300 low-income people on the public housing waitlist. Kallem said the Philly Joy Bank has full support from the city of Philadelphia.
Community input
A Black mother of two, Lydia Seymour, helped develop the pilot program by sharing her lived experience, facilitating workgroups and fundraising.
The Philadelphia Community Action Network introduced her to other moms who provided tips and resources while she was unemployed and pregnant with her second child in 2020. Eventually, the coalition paid her $25 an hour to share insight from her motherhood journey. The additional income covered some basic needs during her pregnancy, said Seymour, who now works as a coordinator for the coalition.
Adverse birth outcomes hit close to home for Seymour, since her daughter was born at an extremely low birth weight — 1 pound, 8 ounces — in 2017. If the guaranteed income program was around at that time, she said it would have made a significant difference for her first pregnancy.
“Across the board in any ethnic background or racial group, finances are seen as a stress and a source of need,” Seymour said. “So having an extra $1,000 during pregnancy would have helped to put food on the table.”
The Philly Joy Bank was also inspired by Manitoba’s Healthy Baby Prenatal Benefit program, which launched in 2001 to improve health outcomes during pregnancy. Recipients of the government-run program receive up to $81.41 (about $60 USD) a month throughout their second and third trimester, depending on their income. Additionally, expectant parents receive access to prenatal care and referrals to a support system where they can, among other things, learn about baby development, connect with other expectant parents, get breastfeeding support or ask questions about pregnancy. To be eligible for the program, expectant parents must have a household income under $32,000 and reside in Manitoba.
From 2001 to 2016, the Manitoba program provided over $27 million in total to around 63,000 women, according to the latest government report. In 2016, over 30% of the beneficiaries lived in First Nations communities.
The unrestricted cash had measurable impacts. Among those: reducing the risk of low birth weights by 21% and preterm births by 17.5%, 2016 research showed.
Study author Marni Brownell, a University of Manitoba professor in community health sciences and senior research scientist at the Manitoba Centre for Health Policy, evaluated the prenatal benefit for children born from 2003 through 2011 and followed them through kindergarten over several studies. In one paper, she found that the benefit led to increased vaccination, as well as improved cognitive and language development among First Nations children.
For jurisdictions that want to implement a similar program, Brownell recommends free prenatal care and efforts to reduce barriers to that service, including a lack of childcare and transportation, as well as distrust of the healthcare system.
In Philadelphia, the pilot program’s recruitment and enrollment process is still underway. The Department of Public Health anticipates holding community events and outreach in childcare centers and prenatal care sites. Philly Joy Bank will be considered for renewal if it improves financial security, as well as maternal and child health outcomes, said Kallem, adding that the city is currently selecting an external evaluator to measure the program’s impact.
In Brownell’s eyes, the research on Manitoba’s program provides a key message: “Women know best what they need to improve their prenatal health.”