By: Sze Yan Liu
See original post here.
The Big Idea
When people living in poverty in countries like Malawi, Indonesia, and Ecuador receive cash payments without having to do anything in return, they have better health, according to a scientific review of a large body of research.
To reach that finding, our interdisciplinary team of public health experts, economists, and epidemiologists from Canada, Germany, New Zealand, and the United States pooled data from 34 studies that involved 1,140,385 participants in 50,095 households across Africa, the Americas, and Southeast Asia.
Our systematic review and meta-analysis also determined that unconditional cash payments in low- and middle-income countries not only reduce poverty, but they also lead to greater food security, improved nutrition, and more consistent school attendance.
Follow-up surveys with individuals who received this money earlier found that they were less likely to have been sick in the previous two weeks to three months compared with individuals who had not received this money. In addition, there is some evidence that people who got cash payments spent more money on health care.
The studies we examined involved 24 cash-payment programs in 13 countries that were run either by governments, nonprofits, or researchers. The value of the money given to people in need varied widely, anywhere from 1.3 percent to 81.9 percent of gross domestic product per capita.
Why It Matters
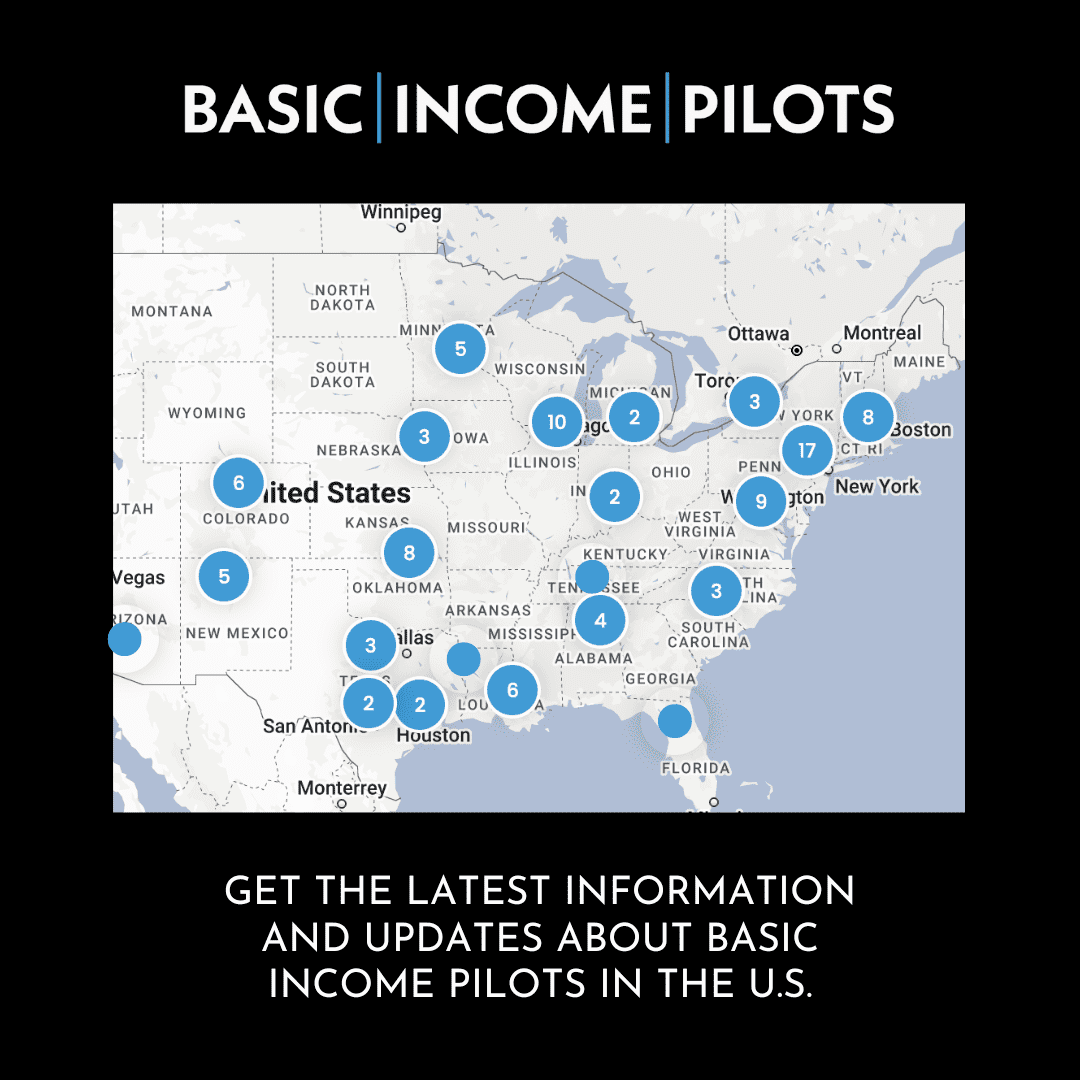
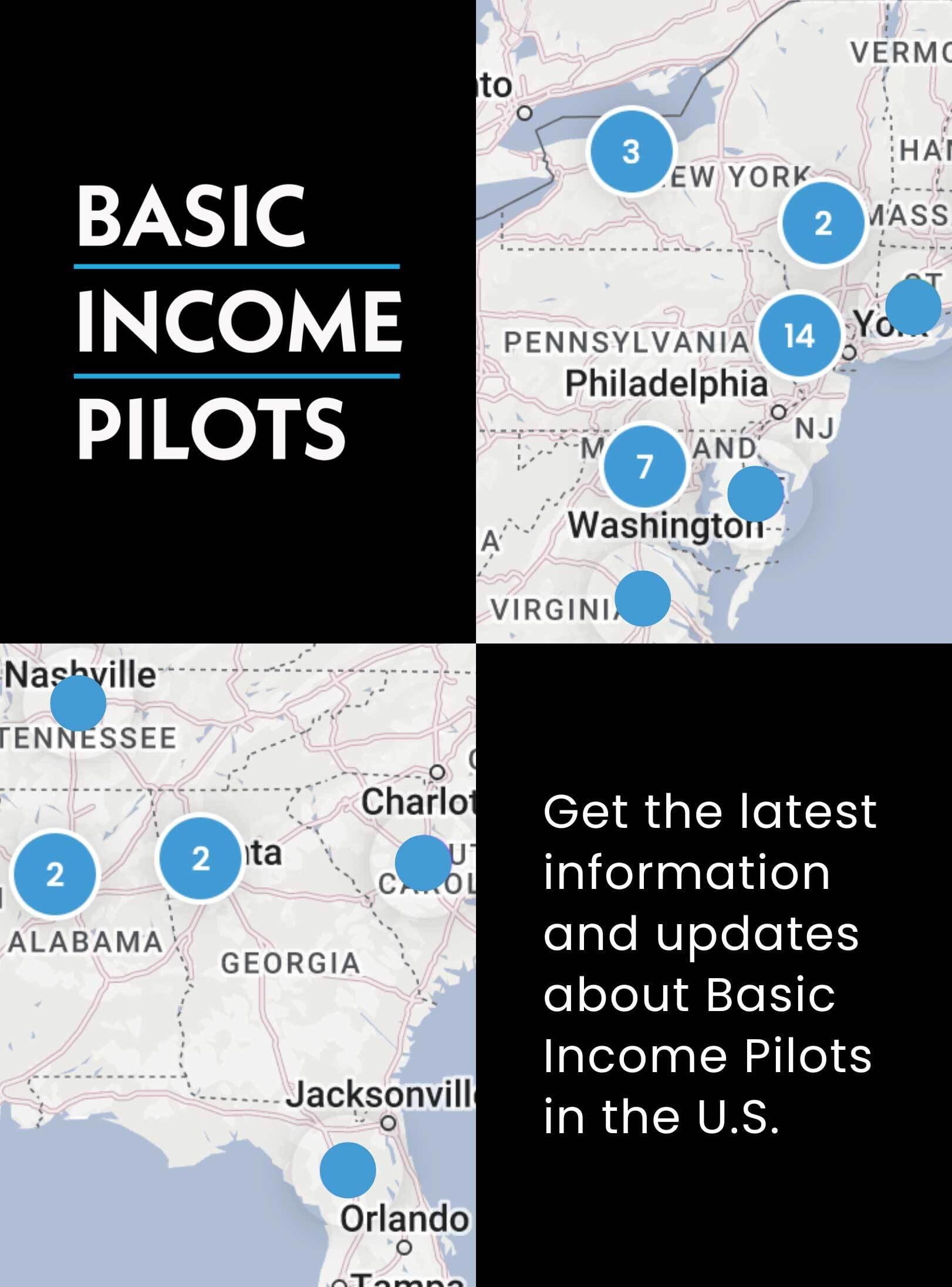
Governments, nonprofits, and researchers around the world are increasingly experimenting with a simple approach to reduce poverty: giving people money to spend on whatever they need.
Many of these cash-transfer pilots and experiments — often called basic-income programs — have required people to do something to receive the money, such as making sure their children regularly attend school. Sometimes the condition involves completing a specific health-related task, such as attending a health education workshop or going to a preventive care medical appointment.
Researchers are debating whether these conditions improve or hinder the effectiveness of these programs.
Other programs, like those we studied, have no such requirements.
One advantage of the no-strings-attached approach, argue the GiveDirectly nonprofit and other supporters, is that it eliminates the need to monitor compliance and slashes administrative costs. Unconditional cash payments may empower recipients more since they can decide how to use the money to meet some of their immediate needs.
Making payments contingent on people meeting requirements may also unintentionally harm people in need who can’t comply with conditions due to physical, social, or economic barriers. For example, requiring a clinic visit to “earn” a cash payment does not help anyone unable to make the trip.
What Still Isn’t Known
We still don’t have enough information to determine if this pattern holds true in the United States and other wealthier nations.
The long-term health benefits of unconditional cash payments is also not clear.
Finally, more research is needed to understand whether the impetus for these programs, such as when they follow a hurricane or other major disaster, makes any difference.
What’s Next
Our team plans to study whether cash-payment programs that require compliance with conditions lead to better health, too. We also want to update a previous review we conducted of payments given to people who had experienced humanitarian disasters to include evaluations of similar efforts carried out during the Covid-19 pandemic.
Editor’s note: This article is part of a partnership the Chronicle has forged with the Conversation to expand coverage of philanthropy and nonprofits. The three organizations receive support for this work from the Lilly Endowment. This article is republished from the Conversation under a Creative Commons license.