See original post here.
I’m a Pediatrician Caring for Families in Poverty. Here’s What’s Been Happening at My Hospital Since the Child Tax Credit Expired.
When it’s my turn to be the pediatrician in the well-baby nursery at my hospital, my job is to counsel new parents about healthy newborn behaviors and assure them their babies are capable of basic survival. Breathing. Eating. Pooping. The rhythm and routine of newborn assessment are rote: look, listen, feel. Healthy babies have commonalities that allows doctors like me to decipher illness from health. When I look, I note each infant has one mouth, two eyes, four limbs wiggling about. I place my stethoscope atop each tiny chest, listening for crisp, clear breaths between rapid, steady heartbeats. I feel each baby’s bones as I run my fingers across clavicles, along spines, atop skulls. I identify with the pure affection manifest as mothers cuddle their children against their chests.
My pediatric colleagues and I apply this same rhythm and routine daily to parse the implications of poverty. I work at a safety-net hospital in Philadelphia. The median household income in the neighborhood outside our hospital’s manicured lawns is $36,572. Most of our insured patients qualify for Medicaid. We have always listened for insecurities related to poverty. Some abated last year when the child tax credit was in effect. Since its expiration in January, however, these stresses have crept back in.
Essentials are again inconsistently attainable. Parents in our clinics increasingly need assistance procuring diapers. Parents in our neonatal intensive care unit (NICU) increasingly request referrals for cribs, for food, for bus passes.
Requests for car seats come in the clinic, the nursery, and the NICU. We replenish the pile of newborn clothes in our hospital’s donation closet each time the pile dwindles, the bins labeled not by what they contain, but by the names of the churches who provided their contents. I again hear parents telling me about taking three buses each way, every day, to visit their hospitalized premature babies, because they cannot afford an Uber.
This is all on top of the nationwide formula shortage, which has the nurse manager in the NICU calling our formula representative constantly, hoping she can source rare formulas for our most fragile patients.
We are buoyed by the village of agencies, policies, public programs, donors, nonprofit organizations, and community members, but it is tempting to feel devastated by the depth of need. That our social worker can provide temporary breast pumps and that our nurse manager can source funds for transportation belies the point. We can find these and other solutions because the rhythms and routines we hear are predictable. But for a while, we did not have to. For months, I did not meet a single new mother pumping breast milk, drop by drop, with her own hands as she waited for her health insurance to deliver an electric pump.
As I walk from room to room, my patients’ bodies appear indistinct. But a study out in April taught me that if I were to look deeper, with tools more sensitive than my own eyes, I might see effects of poverty imprinted inside those bodies. These researchers examined newborn brains with magnetic resonance imaging and found alterations in how brains form and develop in the face of maternal social disadvantage. Put another way, poverty impacts fetal brain growth. Overcoming those effects is certainly possible. Examples abound. But I do not believe any baby should have to try.
Discussing research that differentiates fetuses based on lived experiences of pregnant women can be problematic. Many may be tempted to blame pregnant mothers for the adverse outcomes their children suffer. Mother blaming is not a new concept. The idea that women should be virtuous vessels, capable of perfect pregnancies in the face of societal stressors and systemic racism is a fallacy. No one chooses to live in poverty. Not pregnant women, not children. No one.
And this new data is not surprising.
The link between adverse health outcomes and poverty in pregnancy, infancy, and early childhood is irrefutable.
The seminal report “From Neurons to Neighborhoods” provided cogent and coherent content about poverty’s effect on newborns and young children in 2000. What is surprising is that, in the 22 years since this report, and all the years since the reports that came before it, the pace of progress has been slow.
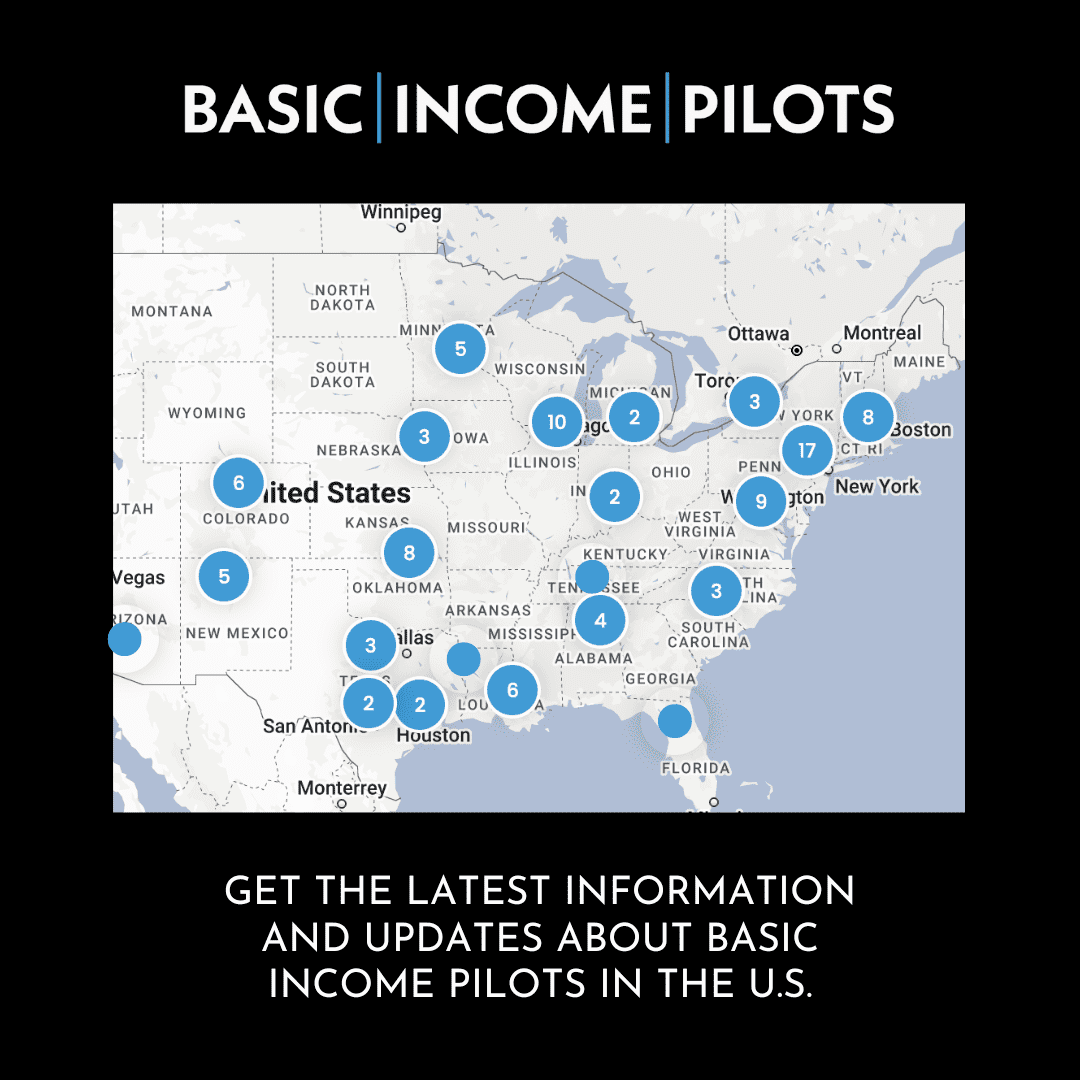
Slow progress is not no progress. The moral imperative to support all citizens to birth healthy babies and raise healthy children is also a financial imperative to ensure healthy adults, healthy citizens. Healthy workers. Pilot programs to provide funding for pregnant women are under way in California. The child tax credit was a cost-effective federal policy that successfully reduced child poverty and uplifted the lives of mothers raising children while pregnant.
I am not an expert on poverty. I have lived my whole life fed and housed. I do not research poverty’s effects like the study authors in St. Louis, nor am I an expert in early child development like those who authored “From Neurons to Neighborhoods.” But I have spent my pediatric career listening to my patients’ parents share their stories after I remove my stethoscope from my ears. Their stories taught me to see beyond what my own eyes may capture, to do all I can to support those I serve.
Not everything improved in the wake of the child tax credit. The early-morning ritual on our postpartum unit of fathers, mindful of disturbing their partners’ sleep, leaving for jobs in warehouses, factories, retail stores, and then returning each evening to participate in newborn bonding they missed while working, never ceased. My colleagues who staff our pediatric and teen clinic serve patients increasingly victimized by gun violence. But in hindsight, we spent less time last year sourcing necessities for our families and could care for our patients in other ways. For a while, our patients’ families spent less energy triaging poverty.
Toward the end of every newborn assessment, I elicit the common reflexes babies require to survive. A startle, a suck, a grasp. When I press my pointer finger atop a newborn’s palm, he predictably grasps my finger. If I do not pull my hand away, his grip persists. Babies, people, are resilient. Our bodies are predestined to grip and grab and hold on to all we are offered. I only wish our nation would place more in each palm.