If medically assisted death becomes more accessible for Canadians, we have a moral obligation to make living well — through housing, mental health supports — accessible too.
Opinion by Naheed Dosani
At the start of the year, the Canadian Senate made it a priority to discuss Bill C-7 on Medical Assistance in Dying (MAID), which proposes to make MAID more accessible for people, even if they don’t have a limited prognosis.
I was asked to testify — to share my perspective as a palliative care physician who provides street-based care for people with serious illnesses who also experience structural vulnerabilities like homelessness, poverty, and systemic racism.
Why is this perspective integral to the discussion about Bill C-7?
I work in a world where it is possible to successfully arrange for MAID in two weeks in an organized and efficient fashion.
Yet, it takes years to get the people I care for into housing, months to get them income supports, and weeks to get mental health and harm reduction treatment essential to a good quality of life.
I find this morally distressing.
If we are making it easier for people to get MAID, we also have a moral obligation to ensure that people don’t pursue MAID because they want to escape a society that doesn’t adequately support their needs.
I think of the people I have cared for over the years, like “Bob,” a man in his 50s with multiple sclerosis and complex wounds. He was referred to our palliative care team for management of complex pain. Despite optimizing his pain and providing expert wound care, he pursued MAID. Why? Because his progressive disease and its complications on his mental health led to an alcohol use disorder, which led to him losing his housing, which led to him losing his family and, ultimately, being alone.
Conversely, I have witnessed how treating the social determinants of health for the people I care for, can make a tremendous difference as to whether-or-not someone pursues MAID. “Mary,” a woman in her 30s, is an example. She was on the streets living with untreated HIV, dealing with a substance use disorder and no health care team to meet her needs. Mary wanted to die through MAID. However, after addressing her emotional and physical pain, supporting her with housing, income, harm reduction services and providing the kind of psychosocial supports that all Canadians deserve, she changed her mind because she now has a better quality of life.
When discussing Bill C-7 & MAID, it is crucial to recognize that all people across Canada do not access palliative care equally.
Further, people who experience structural vulnerabilities like poverty, homelessness and systemic racism face even more barriers to accessing palliative care.
Although it has historically suffered from an identity crisis because of its association with death, palliative care addresses a person’s suffering throughout serious illness — regardless of prognosis.
It considers the whole person — their physical, psychological, social, spiritual, and practical needs. It is an active treatment that focuses on living and can prolong life in some cases.
For several years, experts across Canada have expressed the need to implement a palliative approach to care, as outlined in The Way Forward, and How to improve Palliative Care in Canada. These reports highlight several high-quality and cost-effective approaches to help Canadians with life-threatening illnesses live as fully as possible. Aside from the 2018 release of the Health Canada Framework on Palliative Care in Canada, few recommendations have been fully implemented.
While we have a long way to go to improve access to palliative care services for most Canadians, we have an even longer way to go for those who experience barriers to palliative care due to marginalization.
In 2014, I joined a research team led by Dr. Kelli Stajduhar at the University of Victoria to answer the question: What are the barriers that people on the margins of our society experience in accessing palliative care?
The research study and the report that followed called ‘Too Little Too Late’ tells a damning story.
Through 300 hours of observational research, our team followed 25 homeless and vulnerably housed people with life-limiting disease, their support persons and service providers.
What did we find?
That dying participants bore the brunt of all the commonly experienced injustices lived routinely by people who are structurally vulnerable. That palliative care is harder to access when you are marginalized.
For those who live on the streets:
● The need to survive prevails over discussions about palliative care.
● Death is 2.3-4x more likely, so palliative care is harder to access and initiate.
● Amidst the overdose death crisis, access to palliative care through a trauma-informed harm reduction lens, is difficult to find.
To make palliative care more equitably accessible, we must scale up programs that support people who experience marginalization. We now have many promising practices, including mobile services, harm reduction approaches and trauma-informed care models in cities like Victoria, Edmonton, Calgary and Toronto, that work. Regarding MAID, we need to ask ourselves if we have conducted enough research to reflect the experiences of those who live on the margins. I fear we don’t know enough about these perspectives.
I also worry that Bill C-7 will have a disproportionate impact on working-class disabled people, people who experience homelessness, poverty, and structural marginalization — people who cannot afford their basic needs like food and shelter and medication.
Without investments to end the structures that create these situations, MAID may not be a fair choice for everyone.
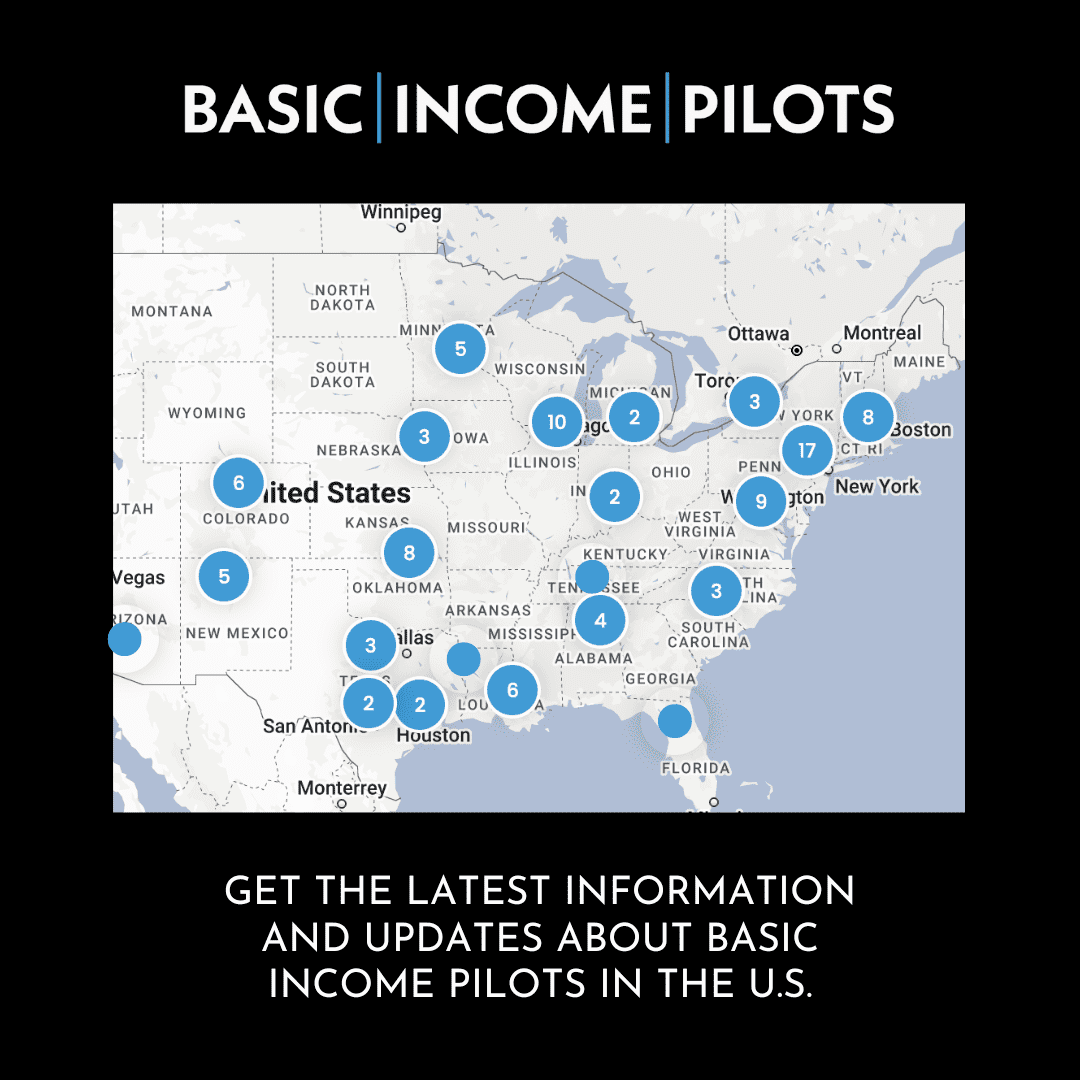
With 35,000 Canadians experiencing homelessness every night, it should be reasonable to expect that the same energy put into passing MAID will also be put into addressing the upstream factors that lead to poor health like a national housing strategy, improving harm reduction services, implementing basic income strategies and pharmacare.
We must do better. It’s a matter of quality of life and death.
_____
Dr. Naheed Dosani is a palliative care physician and health justice advocate who serves as a lecturer at the University of Toronto and an assistant clinical professor at McMaster University. Follow him on Twitter @NaheedD.
To see original article please visit: https://www.thestar.com/opinion/contributors/2021/02/11/if-medically-assisted-death-becomes-more-accessible-for-canadians-we-have-a-moral-obligation-to-make-living-well-through-housing-mental-health-supports-accessible-too.html